With San Diego County moving to the Purple Tier, and new restrictions effective November 14, 2020, you’re likely closely monitoring the local COVID-19 numbers. These numbers are the metrics used by state and local authorities when determining which
businesses and activities can open and which restrictions should be enforced.
Here’s what the numbers really mean and why they’re so important.
Understanding state guidelines
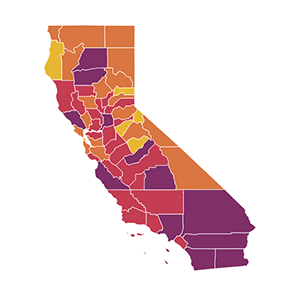 In California, state authorities use a four-tier, color-coded system — ranging from minimal
spread of the disease to widespread — to determine whether a community is in the position to safely open businesses and other activities. California counties must stay in a tier for at least three weeks before being moved to a less restrictive
tier, and will be moved to a more restrictive tier if metrics worsen for two consecutive weeks.
In California, state authorities use a four-tier, color-coded system — ranging from minimal
spread of the disease to widespread — to determine whether a community is in the position to safely open businesses and other activities. California counties must stay in a tier for at least three weeks before being moved to a less restrictive
tier, and will be moved to a more restrictive tier if metrics worsen for two consecutive weeks.
The state focuses on the following numbers to make a determination:
New cases: This number represents the daily number of confirmed COVID-19 cases per 100,000 people. If more than an average of 7 out of 100,000 people test positive each day of a seven-day period, the state would consider this “widespread.”
On the other end of the spectrum, an average of less than one new daily case per 100,000 puts the county in the “minimal” tier, allowing most indoor business operations to be open with modifications.
Positive tests: This number is determined by looking at the number of COVID-19 tests with a positive result out of the total number of tests performed over a seven-day period. For example, if 100 tests are performed and 6 of those tests are confirmed
positive, the percentage is 6%. California classifies a county’s risk level as minimal if less than 2% of tests are positive, and widespread if more than 8% are positive.